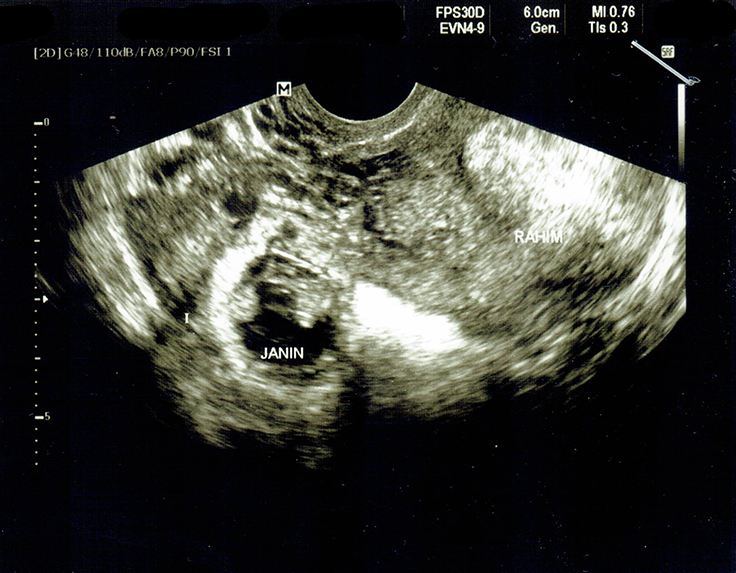
Pregnancy is a transformative journey marked by unique physical and emotional changes, and one aspect that often comes to the forefront is cravings. While cravings during pregnancy are common and can be influenced by hormonal fluctuations, striking a balance between indulging in cravings and maintaining optimal nutrition is essential for the health of both the mother and the developing baby. This delicate equilibrium requires an understanding of the nutritional needs during pregnancy, the reasons behind cravings, and making informed choices to support overall well-being.
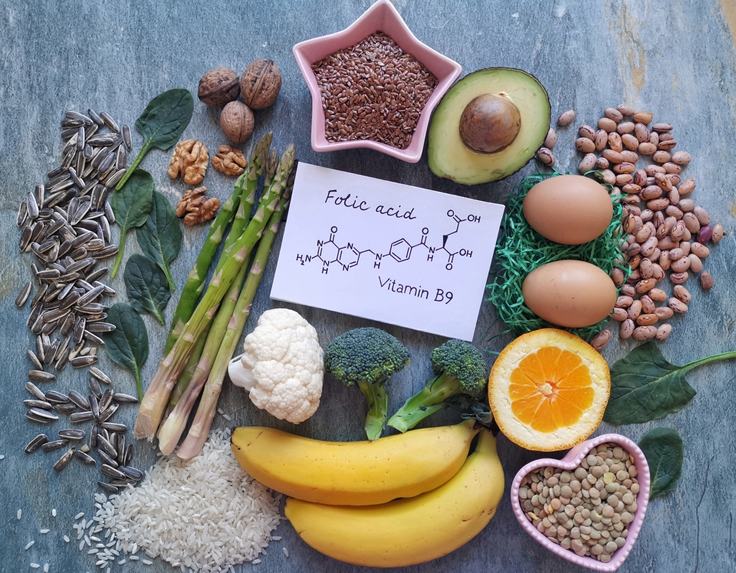
Pregnancy is a time of increased nutritional demands to support the growth and development of the baby. Essential nutrients such as folic acid, iron, calcium, protein, and omega-3 fatty acids play crucial roles in fetal development, organ formation, and overall maternal health. Meeting these nutritional requirements is vital for a healthy pregnancy and can positively influence the long-term health of both the mother and the child.
Why are pregnancy cravings important?
Pregnancy cravings are important for several reasons, and while they might seem like strange desires for specific foods, they often serve as signals that can provide insights into the nutritional and emotional needs of the expectant mother. Here are some reasons why pregnancy cravings are considered important:
Nutrient Signaling: Cravings during pregnancy may be the body’s way of signalling a need for specific nutrients. For example, a craving for certain fruits may indicate a need for vitamin C, while a desire for dairy products may suggest a requirement for calcium. Paying attention to these cravings can help mothers address nutritional deficiencies and support the healthy development of the baby.
Hormonal Changes: Hormonal fluctuations during pregnancy can influence taste preferences and cravings. For instance, changes in levels of hormones like estrogen and progesterone may impact the sense of taste, leading to an increased or decreased preference for certain flavours. Understanding these hormonal shifts can help expectant mothers navigate their changing appetites.
Meeting Increased Caloric Needs: Pregnancy is associated with an increase in energy and nutrient requirements to support the growth and development of the baby. Cravings may be the body’s way of signalling a need for additional calories or specific nutrients necessary for fetal development and overall maternal health.
Addressing Emotional Needs: Cravings are not solely driven by physical needs; they can also be influenced by emotional factors. Pregnancy is a time of significant emotional and psychological changes, and cravings may offer a way for expectant mothers to cope with stress, anxiety, or other emotional challenges. Understanding and addressing these emotional aspects can contribute to overall well-being.
Variety in Diet: Cravings often lead individuals to diversify their diets, introducing a range of flavours and nutrients. This variety can be beneficial in ensuring that the expectant mother is consuming a well-rounded and balanced diet, providing essential nutrients for both herself and the developing baby.
Enjoyment of Food: Pregnancy cravings can be an enjoyable aspect of the pregnancy experience. They allow expectant mothers to indulge in foods they may not typically consume, promoting a positive relationship with food during a time when dietary restrictions are often lifted.
While pregnancy cravings can provide valuable insights, it’s important to approach them with balance and moderation. Not all cravings need to be indulged in excessively, and it’s essential to prioritize a well-balanced and nutrient-dense diet. Consulting with healthcare providers can help expectant mothers make informed choices, ensuring that both cravings and nutritional needs are addressed for a healthy pregnancy.
How can balance your meal that effectively satisfies both cravings and nutritional needs?
Balancing meals to effectively satisfy both cravings and nutritional needs during pregnancy involves thoughtful planning and making choices that prioritize nutrient-dense foods while accommodating specific taste preferences. Here are some strategies to achieve this balance:
- Ensure that your meals include a variety of food groups, including fruits, vegetables, whole grains, lean proteins, and dairy or dairy alternatives.
- Each food group provides different essential nutrients, helping to meet a broad spectrum of nutritional needs.
- Pay attention to your cravings, but practice moderation. You can include the foods you crave in your meals, but try to balance them with other nutrient-rich options.
- For example, if you’re craving something sweet, pair it with a source of protein or fibre to enhance overall nutritional value.
- Choose nutrient-dense foods that provide a high concentration of vitamins and minerals without excess calories. Examples include leafy greens, berries, nuts, seeds, and lean proteins. These foods help ensure you’re getting essential nutrients while keeping your overall calorie intake in check.
- Protein is essential for the growth and development of the baby and helps keep you feeling satisfied.
- Choose whole grains over refined grains to increase the fibre content of your meals. Whole grains, such as brown rice, dalia, and whole wheat, provide essential nutrients and contribute to digestive health.
- Incorporate sources of healthy fats, such as makhana, nuts, seeds, and olive oil. These fats are important for brain development and can help satisfy cravings for rich or creamy textures.
- Drink plenty of water throughout the day. Sometimes, cravings may be linked to dehydration, so staying well-hydrated can help manage cravings effectively.
- Discuss your cravings and dietary choices with your healthcare providers. They can offer personalized advice based on your individual health status, nutritional needs, and any specific concerns.
- Plan balanced snacks that combine protein, carbohydrates, and healthy fats. This can help manage cravings between meals and provide sustained energy.
- Examples include yoghurt with fruit, whole-grain crackers with cheese, or a small smoothie with protein.
Practice mindful eating by paying attention to hunger and fullness cues. This can help prevent overeating and promote a healthy relationship with food. Remember that pregnancy is a unique and individual experience, and what works for one person may not work for another. It’s essential to prioritize both enjoyment and nutritional value in your meals, and consulting with healthcare providers or a registered dietitian can provide tailored guidance to meet your specific needs.

Impact of cravings on nutrition
The impact of cravings on nutrition during pregnancy can be both complex and varied. While cravings are a common and natural phenomenon, they can influence dietary choices and potentially impact overall nutritional intake. Understanding the interplay between cravings and nutrition is essential for expectant mothers to ensure a well-balanced diet that meets both their taste preferences and the nutritional needs of themselves and their developing babies. Here are some key considerations regarding the impact of cravings on nutrition during pregnancy:
- Cravings can strongly influence the types of foods a pregnant woman desires and chooses to consume. These cravings may lead to an increased intake of certain foods, sometimes ones that are rich in sugars, fats, or salt.
- While some cravings may align with the body’s need for specific nutrients, others might be for less nutritious foods. For example, cravings for sweets may be linked to a desire for quick energy, but consistently indulging in sugary treats can lead to an imbalance in nutrient intake.
- Balancing cravings with nutrient-dense food choices is crucial. Incorporating a variety of fruits, vegetables, whole grains, lean proteins, and healthy fats can help ensure that overall nutritional needs are met.
- Practising moderation is key when addressing cravings. Indulging in craving-related foods in appropriate portions allows for enjoyment without compromising overall nutritional balance.
- Cravings for certain foods may be influenced by dehydration. Ensuring an adequate intake of water can help manage cravings and prevent unnecessary consumption of calorie-dense snacks.
- Uncontrolled and excessive indulgence in cravings, especially those for foods high in sugars and fats, can contribute to excessive weight gain during pregnancy. Managing portions and making nutrient-rich choices can help control weight gain while satisfying cravings.
- Cravings may also have emotional components, and the desire for specific comfort foods can be linked to emotional well-being. It’s important to address emotional needs without solely relying on less nutritious food options.
- Some pregnant individuals may experience cravings for foods that are restricted due to dietary concerns or cultural practices. Striking a balance between honouring cravings and adhering to dietary restrictions is essential.
Expectant mothers should discuss their cravings and dietary choices with healthcare providers. Healthcare professionals can provide guidance based on individual health status, nutritional needs, and any concerns related to cravings.
Mindful Eating:
While cravings are a normal part of pregnancy, their impact on nutrition can vary. Striking a balance between satisfying cravings and maintaining a well-rounded, nutrient-dense diet is crucial for supporting both maternal and fetal health. Seeking guidance from healthcare providers or a registered dietitian can help individuals make informed choices that align with their unique nutritional requirements during pregnancy.
FAQs
- What is a healthy pregnancy craving?
A healthy pregnancy craving typically involves a desire for nutrient-dense foods that provide essential vitamins, minerals, and macronutrients necessary for the well-being of both the expectant mother and the developing baby. Examples of healthy pregnancy cravings may include fresh fruits, vegetables, whole grains, lean proteins, and dairy products. These cravings align with the body’s increased nutritional needs during pregnancy and contribute to a balanced and wholesome diet.
- What happens if you ignore pregnancy cravings?
Ignoring pregnancy cravings does not have serious consequences as long as the overall diet remains balanced and meets nutritional requirements. Cravings are often influenced by hormonal changes and taste preferences, and not every craving needs to be indulged in excess. However, if a particular craving persists or if there are concerns about nutritional intake, it is advisable to consult with healthcare providers or a registered dietitian for guidance. They can provide personalized advice based on the individual’s health status and dietary needs during pregnancy.
- What is the importance of nutrition during pregnancy?
Nutrition during pregnancy is critically important for several reasons:
Fetal Development: Adequate nutrition provides essential nutrients for the proper growth and development of the baby’s organs, tissues, and overall body structure.
Maternal Health: Proper nutrition supports the health and well-being of the expectant mother, helping to prevent nutrient deficiencies and complications such as gestational diabetes and preeclampsia.
Immune Support: A well-balanced diet contributes to a strong immune system, helping both the mother and the baby resist infections and illnesses.
Prevention of Birth Defects: Certain nutrients, such as folic acid, play a crucial role in preventing neural tube defects and other birth abnormalities.
Energy for Pregnancy Demands: Pregnancy increases energy requirements, and a nutritious diet provides the necessary calories and nutrients to meet these increased demands.
Reduced Risk of Complications: Proper nutrition can help reduce the risk of complications during pregnancy, including low birth weight, preterm birth, and developmental issues.
Postpartum Recovery: Adequate nutrition sets the foundation for a healthy postpartum recovery, supporting breastfeeding and replenishing nutrient stores depleted during pregnancy.
Overall, maintaining a well-balanced and nutrient-dense diet during pregnancy is crucial for the health of both the mother and the baby. Consulting with healthcare providers or a registered dietitian can ensure that individual nutritional needs are met and contribute to a positive and healthy pregnancy experience.