Embarking on the journey of family planning often involves meticulous tracking of fertility, with ovulation tests emerging as valuable tools for predicting the most fertile window in a woman’s menstrual cycle. However, the accuracy of these tests can be influenced by various factors, including medications. The interplay between medications and ovulation test results raises questions about the reliability of these tests in the presence of pharmaceutical influences.
Ovulation tests play a pivotal role in aiding individuals and couples on their fertility journey by helping predict the optimal window for conception. However, the reliability of these tests can be influenced by a variety of factors, and medications are among the key variables that may impact the accuracy of ovulation test results.
What are ovulation test kits?
Ovulation test kits, also known as ovulation predictor kits (OPKs), are tools designed to help individuals, especially women, identify their most fertile days within the menstrual cycle. These kits detect the surge in luteinizing hormone (LH) that occurs just before ovulation. Ovulation is the process where a mature egg is released from the ovary, making it available for fertilization by sperm.
Here’s how ovulation test kits typically work:
Luteinizing Hormone (LH) Surge: In the middle of the menstrual cycle, there is a surge in LH, which is a key indicator that ovulation is about to occur. This surge usually happens approximately 24-48 hours before ovulation.
Test Strips: Ovulation test kits consist of test strips or devices that are designed to detect the presence of LH in urine.
Testing Procedure: To use an ovulation test kit, an individual typically collects a urine sample and applies it to the test strip or device according to the kit’s instructions. The LH surge, if present, will be indicated by a change in colour or a symbol on the test.
Result Interpretation: A positive result on the ovulation test indicates that the LH surge has been detected, suggesting that ovulation is likely to occur within the next one to two days. This is considered the most fertile period of the menstrual cycle.
Timing Intercourse: Knowing when ovulation is likely to happen allows couples to time intercourse for the days when conception is most likely.
It’s important to note that while ovulation tests can be a helpful tool for predicting fertile days, they do not confirm whether ovulation actually occurred or guarantee pregnancy. They are most effective when used in conjunction with other methods of fertility awareness and family planning.
Ovulation test kits are readily available over-the-counter at pharmacies and online, making them a convenient option for individuals who are actively trying to conceive or who want to understand their menstrual cycles better. As with any medical or fertility-related tool, it’s advisable to follow the instructions carefully and consult with a healthcare professional if there are any concerns or questions about fertility tracking.

Effect of medication on Ovulation test result
The accuracy of ovulation test results can be influenced by certain medications, as these drugs may affect the hormonal processes that the tests rely on to detect the surge in luteinizing hormone (LH). LH is a key hormone that triggers ovulation, and ovulation tests work by identifying this surge to predict when ovulation is likely to occur. Here are some ways in which medications can impact ovulation test results:
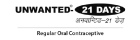
Hormonal Medications: Some hormonal medications, such as birth control pills containing synthetic hormones like estrogen and progesterone, can influence the hormonal fluctuations that ovulation tests are designed to detect. These medications may suppress the natural LH surge, leading to a potential lack of or diminished signal on the ovulation test.
Fertility Medications: Women undergoing fertility treatments may be prescribed medications to stimulate ovulation, such as human chorionic gonadotropin (hCG) or fertility drugs like clomiphene citrate. These medications can elevate LH levels, potentially causing a false positive on ovulation tests. In such cases, the test may detect the exogenous hormones used in fertility treatments rather than the body’s natural LH surge.
Steroids: Corticosteroids, often prescribed for inflammatory conditions, autoimmune disorders, or allergies, can interfere with normal hormonal patterns. This interference may affect the accuracy of ovulation test results.
Anti-inflammatory Drugs: Nonsteroidal anti-inflammatory drugs (NSAIDs), commonly used for pain relief and to reduce inflammation, may also have an impact on ovulation. NSAIDs can potentially disrupt hormonal signalling, affecting the reliability of ovulation tests.
It’s important for individuals using ovulation tests to be aware of any medications they are taking and to consult with healthcare providers about potential interactions. False positives or negatives on ovulation tests can lead to inaccurate predictions of fertility, potentially affecting family planning decisions.
Despite the potential influence of medications, ovulation tests can still provide valuable insights when used carefully and in conjunction with an understanding of individual health and medication regimens. Seeking guidance from healthcare professionals and discussing concerns about medications’ impact on fertility tracking can help individuals navigate the complexities of family planning with greater accuracy and confidence.
Advantages & disadvantages of medications on ovulation test result
Advantages of Medications on Ovulation Test Results:
Facilitation of Ovulation: Fertility medications, such as those used in assisted reproductive technologies or fertility treatments, can help induce or regulate ovulation. In such cases, ovulation tests may serve as a valuable tool to confirm the effectiveness of the medication in triggering ovulation.
Monitoring Treatment Success: For individuals undergoing fertility treatments, medications like human chorionic gonadotropin (hCG) or clomiphene citrate are often used to stimulate ovulation. Ovulation tests can be employed to monitor the success of these treatments, ensuring that ovulation is occurring as expected.
Increased Precision in Timing Intercourse: Medications that enhance the predictability of ovulation can provide couples with a more precise window for timing intercourse. This may be particularly beneficial for those actively trying to conceive, improving the chances of successful fertilization.
Disadvantages of Medications on Ovulation Test Results:
False Positives: Certain fertility medications, especially those containing hormones similar to luteinizing hormone (LH), may lead to false positives on ovulation tests. This is because the test may detect the exogenous hormones from the medication rather than the body’s natural LH surge, potentially confusing predicting ovulation.
Suppression of Natural LH Surge: Hormonal medications, such as birth control pills or hormonal therapies, may interfere with the natural LH surge. This interference can result in a lack of or a diminished signal on ovulation tests, making it challenging to accurately predict ovulation.
Inaccurate Timing for Natural Ovulators: For women not undergoing fertility treatments, certain medications that interfere with hormonal balance (e.g., antidepressants, antipsychotics, steroids) may disrupt the reliability of ovulation test results. This can lead to inaccurate timing for those who rely on these tests to identify their natural fertile window.
Complexity in Interpretation: When medications are involved, interpreting ovulation test results becomes more complex. Differentiating between a genuine LH surge and the influence of medication may require careful consideration and possibly consultation with healthcare professionals.
While medications can play a crucial role in facilitating or regulating ovulation, they can also introduce complexities in interpreting ovulation test results. Understanding the specific impact of medications and seeking guidance from healthcare providers can help individuals navigate the use of ovulation tests more effectively, ensuring accurate predictions and informed family planning decisions.
FAQs
- Can medication delay ovulation?
Yes, certain medications can potentially impact ovulation. It’s crucial to consult with a healthcare professional if you’re taking medications and concerned about their effects on ovulation.
- When is the best time to use the Ovulation Test?
The best time to use an Ovulation Test is typically in the middle of your menstrual cycle. This is usually around 10 to 14 days before the start of your next period. However, individual cycle lengths may vary, so it’s advisable to follow the instructions provided with the specific ovulation test you are using.
- What medications affect ovulation tests?
Several medications can influence ovulation test results. These may include hormonal medications such as birth control pills or fertility treatments. It’s important to inform your healthcare provider about any medications you are taking, as they can guide how these might impact ovulation tests and overall reproductive health.