An ectopic pregnancy is a condition that occurs when a fertilized egg implants outside of the uterus. The most common location for an ectopic pregnancy is in the fallopian tube, but it can also occur in the ovary, cervix, or abdomen. Ectopic pregnancies cannot survive and can be life-threatening if not treated promptly.
Symptoms of an ectopic pregnancy include abdominal or pelvic pain, light vaginal bleeding, and tenderness in the abdomen. If left untreated, an ectopic pregnancy can cause the fallopian tube to rupture, leading to internal bleeding and the need for emergency surgery.
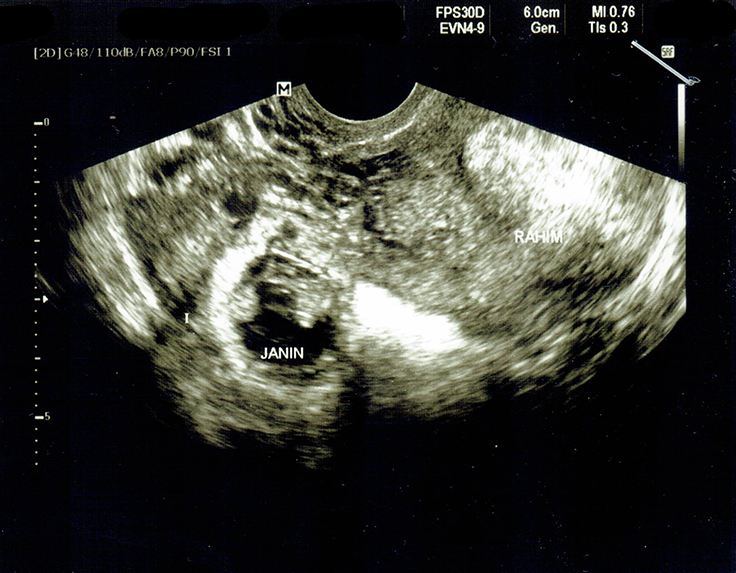
Diagnosis of an ectopic pregnancy is typically made through a combination of physical examination, blood tests, and imaging studies, such as an ultrasound. Treatment options include medication (such as methotrexate) to stop the growth of the pregnancy, or surgery to remove the pregnancy.
It is important for women who are at risk for an ectopic pregnancy to receive early and regular prenatal care to ensure prompt diagnosis and treatment. Women who have had an ectopic pregnancy may also be at increased risk for future ectopic pregnancies and should be monitored closely during any future pregnancies.
What causes an ectopic pregnancy?
The exact cause of ectopic pregnancies is not well understood, but several risk factors have been identified.
One of the most common causes of ectopic pregnancy is a pelvic inflammatory disease (PID), which is an infection of the reproductive organs. PID can cause inflammation and scarring in the fallopian tubes, making it difficult for the fertilized egg to pass through to the uterus.
Another risk factor for ectopic pregnancy is a history of the condition. Women who have had an ectopic pregnancy in the past are at a higher risk of having another one in the future.
Infertility, smoking, and the use of assisted reproductive technologies (ART) such as in vitro fertilization (IVF) can also increase the risk of ectopic pregnancy. These conditions can affect the function of the fallopian tubes and make it more difficult for the fertilized egg to reach the uterus.
Certain congenital conditions such as having a history of tubal surgery, pelvic surgery and congenital tubal abnormalities can also cause an ectopic pregnancy. Hormonal imbalances and structural abnormalities of the uterus, such as a septate uterus, can also contribute to the development of an ectopic pregnancy.
However, it is important for women who are at risk of an ectopic pregnancy to receive regular prenatal care to ensure that the condition is identified and treated promptly, as ectopic pregnancies cannot survive and can be life-threatening if left untreated.
Ectopic pregnancy diagnosis and treatment
One of the first diagnostic tests for ectopic pregnancy is a blood test to measure the levels of a hormone called human chorionic gonadotropin (hCG), which is produced during pregnancy. If the hCG levels are higher than expected, it may indicate an ectopic pregnancy.
Ultrasoun3ed is also used to diagnose ectopic pregnancy, which can help to identify the location of the fertilized egg. In some cases, a transvaginal ultrasound may be performed, which uses a wand-like device inserted into the vagina to obtain images of the fallopian tubes and uterus.
Once an ectopic pregnancy is diagnosed, the treatment options depend on the location of the fertilized egg, the size of the pregnancy, and the overall health of the woman.
In some cases, medication can be used to stop the growth of the pregnancy, but if the pregnancy is too advanced or the fallopian tube is at risk of rupture, surgery is required. Surgery may involve the removal of the fallopian tube in which the ectopic pregnancy is located, called salpingectomy.
After treatment, close follow-up is crucial, with regular blood tests and ultrasound to ensure that the ectopic pregnancy has been resolved. Women who have had an ectopic pregnancy may also be at increased risk for future ectopic pregnancies and should be monitored closely during any future pregnancies.
What are the symptoms of an ectopic pregnancy?
The symptoms of ectopic pregnancy can be similar to those of a normal pregnancy, such as missed periods, breast tenderness, and nausea. However, there are also specific symptoms to look out for, such as:
- abdominal pain or cramping
- shoulder pain
- vaginal bleeding or spotting
- dizziness or fainting
It’s important to note that these symptoms can also occur in a normal pregnancy, so it’s important to seek medical attention if you experience any of them at power.
In addition to these, it is also important to address some frequently asked questions about ectopic pregnancies.
How is an ectopic pregnancy diagnosed?
An ectopic pregnancy is usually diagnosed by a combination of methods including ultrasound, blood tests and pelvic examination.
How early in a pregnancy is an ectopic pregnancy detected?
An ectopic pregnancy can be diagnosed as early as 4-6 weeks after the last menstrual period, but it is usually diagnosed around 7-8 weeks.
Can I get pregnant again after an ectopic pregnancy?
It is possible to get pregnant again after an ectopic pregnancy, but it is important to talk to your doctor about any risks or concerns.
In conclusion, ectopic pregnancy is a serious condition that occurs when a fertilized egg implants outside of the uterus. It can be diagnosed using ultrasound, and treatment depends on the size of the pregnancy and the health of the mother. It is important to be aware of the symptoms of ectopic pregnancy and to seek medical attention if you experience any of them. With proper care and treatment, it is possible to have a successful pregnancy after an ectopic pregnancy.